If you’re worried about whether you’re able to get the COVID-19 vaccine, the Ministry of Health (MOH) had further eased vaccination guidelines so that more people will be able to take the vaccine. Hooray!
MOH updated its guidelines last Saturday (13 Mar), specifically citing the mRNA-based COVID-19 vaccines (aka what we have in stock—the Pfizer-BioNTech and Moderna COVID-19 vaccines).
This comes in addition to the very useful MOH infographic that they posted on Facebook on 10 March, which you should definitely check out below. It lists down the various common medical conditions in Singapore and whether people afflicted with them are able to take the vaccine.
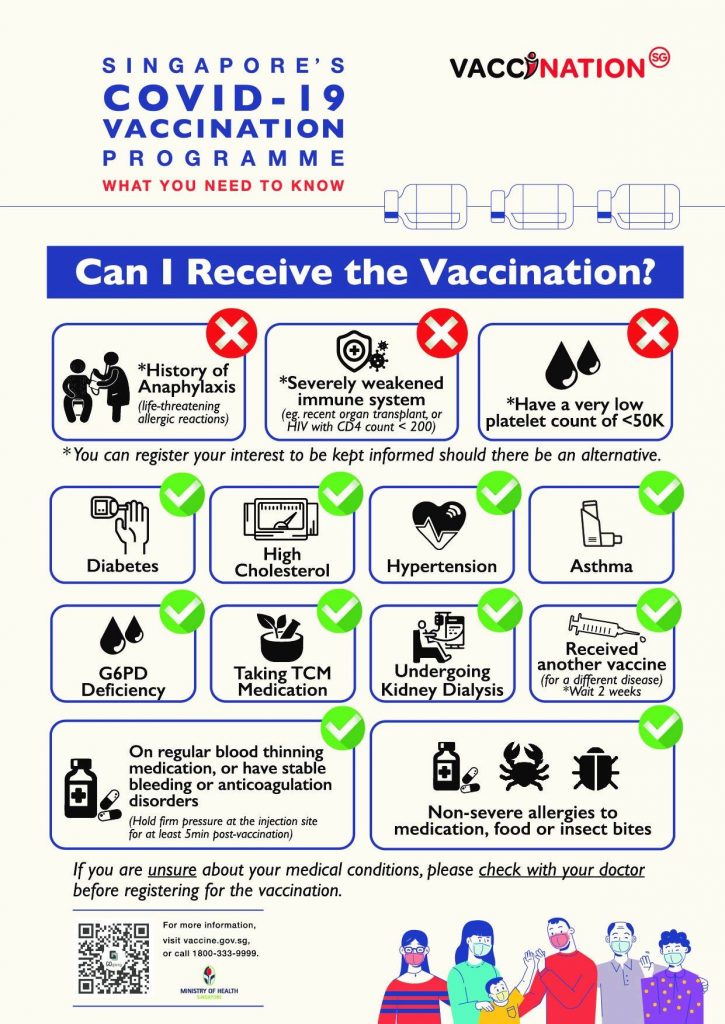
Who Cannot Receive the Vaccine?
As MOH had previously stated, only those with a history of anaphylaxis—a type of life-threatening allergic reaction—cannot receive the COVID-19 vaccine. It has two of the following three criteria:
- Hives or swelling in the face, eyelids, lips or throat
- Difficulty breathing
- Dizziness.
According to MOH’s website, those with a history of having been prescribed an EpiPen suggests an anaphylaxis risk and such persons should not receive the vaccine at this time.
In addition, those who have experienced allergic reactions to the Pfizer-BioNTech or Moderna COVID-19 vaccine, or any other type of vaccines should also not be vaccinated. The latter should consult with specialists to evaluate their suitability.
MOH also said that persons with a history of these severe drug reactions should not be vaccinated either:
- Stevens-Johnsons Syndrome (SJS)
- Toxic Epidermal Necrolysis (TEN)
- Drug Rash with Eosinophilia and Systemic Symptoms (DRESS)
- Drug-induced Hypersensitivity Syndrome (DiHS)
The other two conditions that prevent people from taking the vaccine still stand:
- Those with severely weakened immune system (e.g. recent organ transplant or HIV with CD4 count < 200)
- And those with a very low platelet count of lesser than 50,000
The ministry also elaborated on immunocompromised persons last Saturday, stating that they will be assessed by medical personnel at vaccination centres on their suitability to receive the vaccine. Such persons include those who had:
- A transplant within the past 3 months (solid organ or stem cell)
- Cancer chemotherapy, immunotherapy, or radiation therapy
- Aggressive immunotherapy (e.g. Rituximab) for non-cancer conditions
- HIV infection with CD4 < 200 cells/mL
Other Types of Allergies
Apart from those with anaphylaxis, people with atopy (such as eczema, allergic rhinitis or asthma) can be vaccinated.
Even those with a family history of anaphylaxis, but do not have it themselves, can also receive the mRNA-based vaccines.
As reported by CNA, MOH noted that it is “the severity of the allergy, and not the number of allergies that determines if a person can be vaccinated.”
“[E]merging local and international scientific evidence had shown individuals with NSAIDs-induced angioedema can be vaccinated with a mRNA-based COVID-19 vaccines, as long as there are no other life-threatening signs and symptoms suggestive of anaphylaxis.”
Cancer Patients
Those with active cancer but are not on treatment with chemotherapy, radiotherapy, or immunotherapy can be vaccinated, according to MOH. More specifically, this refers to those who have not been on the above treatments for the past 3 months and have not planned for such treatment in the next 2 months.
Vaccinations can also be carried out on those on active cancer hormonal therapy, or who are in remission.
Other Concerns
MOH also advised those who have recovered from COVID-19 and have not completed their vaccination to take up a single dose in order to “further boost the immunity against COVID-19 in persons who have recovered from a COVID-19 infection.”
Advertisements
Recovered persons should consult their doctor on when to receive the vaccine and the ideal timing would be to wait at least 6 months after their infection.
Mothers who are breastfeeding can also be vaccinated but should take precaution by considering suspending breastfeeding for 5 to 7 days after receiving the vaccine.
Be sure to read MOH’s FAQ on the safety and efficacy of the COVID-19 vaccines if you have any more concerns about your condition.
Feature Image: Miriam Doerr Martin Frommherz / Shutterstock.com
Read Also:
- Real Mercs Driver in Tampines Accident Responded; Said He Sped Up to See Saab’s Car Plate Number
- If You’re a PME, Here’s Another Reason Why You Should Join a Union
- TikTok CEO Chew Shou Zi Responds to TikTok Ban; Confident to Win Legal Challenge
- Popular Peach Garden in Thomson Plaza Suspended After 43 People Allegedly Had Food Poisoning After Eating There
- Driver in Tampines Accident Engaging Lawyer After Being Charged
Advertisements